Prehospital predictors of neurological outcomes in out-of-hospital cardiac arrest patients aged 95 years and older: A nationwide population-based observational study
outcomes in out-of-hospital cardiac arrest patients aged 95 years and older: A nationwide population-based observational study
Funada A, Goto Y, Maeda T, Tada H, Teramoto R, Tanaka Y, Hayashi K, Yamagishi M.
J Cardiol. 2017 Jan;69(1):340-344. ![]()
Impact Factor (2016): 2.732
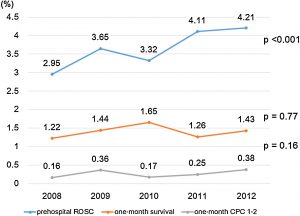
2008~2012年の総務省消防庁全国前向きウツタイン登録の解析から、95歳以上の超高齢院外心停止患者の神経学的転帰は一般に不良であるが、病院到着前にROSC(自己心拍再開)が達成された場合、救急隊による心停止の目撃があった場合には神経学的転帰良好の割合が高いことを報告しました。
Abstract
BACKGROUND:
Population aging has rapidly progressed in Japan. However, few data exist regarding the characteristics of extremely elderly patients with out-of-hospital cardiac arrest (OHCA). We aimed to determine the prehospital predictors of one-month survival with favorable neurological outcomes (Cerebral Performance Category scale, category 1 or 2; CPC 1-2) in this population.
METHODS:
We investigated 23,520 OHCA patients aged ≥95 years from a prospectively recorded, nationwide, Utstein-style Japanese database between 2008 and 2012. The primary study endpoint was one-month CPC 1-2 after OHCA.
RESULTS:
The one-month CPC 1-2 rate was 0.27% (63/23,520). Only two variables were significantly associated with one-month CPC 1-2 in a multivariate logistic regression model: prehospital return of spontaneous circulation (ROSC) [adjusted odds ratio (aOR), 94.4; 95% confidential interval (CI), 50.1-191.7] and emergency medical service (EMS)-witnessed arrest (aOR, 5.1; 95% CI, 2.6-10.2). When stratified by these two predictors, the one-month CPC 1-2 rates were 20.2% (18/89) for patients who had both prehospital ROSC and EMS-witnessed arrest, 4.2% (33/783) for those who had prehospital ROSC without EMS-witnessed arrest, 0.28% (3/1065) for those who had EMS-witnessed arrest without prehospital ROSC, and 0.04% (9/21,583) for those who had neither predictor, respectively.
CONCLUSIONS:
The crucial prehospital predictors for one-month CPC 1-2 in elderly OHCA patients aged ≥95 years in Japan were prehospital ROSC and EMS-witnessed arrest and the former was the predominant predictor.